Introduction
Artificial intelligence is steadily gaining ground in healthcare. Tools that once felt experimental are now helping reduce administrative burdens, improve patient engagement, and enhance revenue cycle performance. Ambient scribes capture clinical conversations in real time, predictive models identify at-risk patients before problems escalate, and automated billing systems prevent denials before they happen.
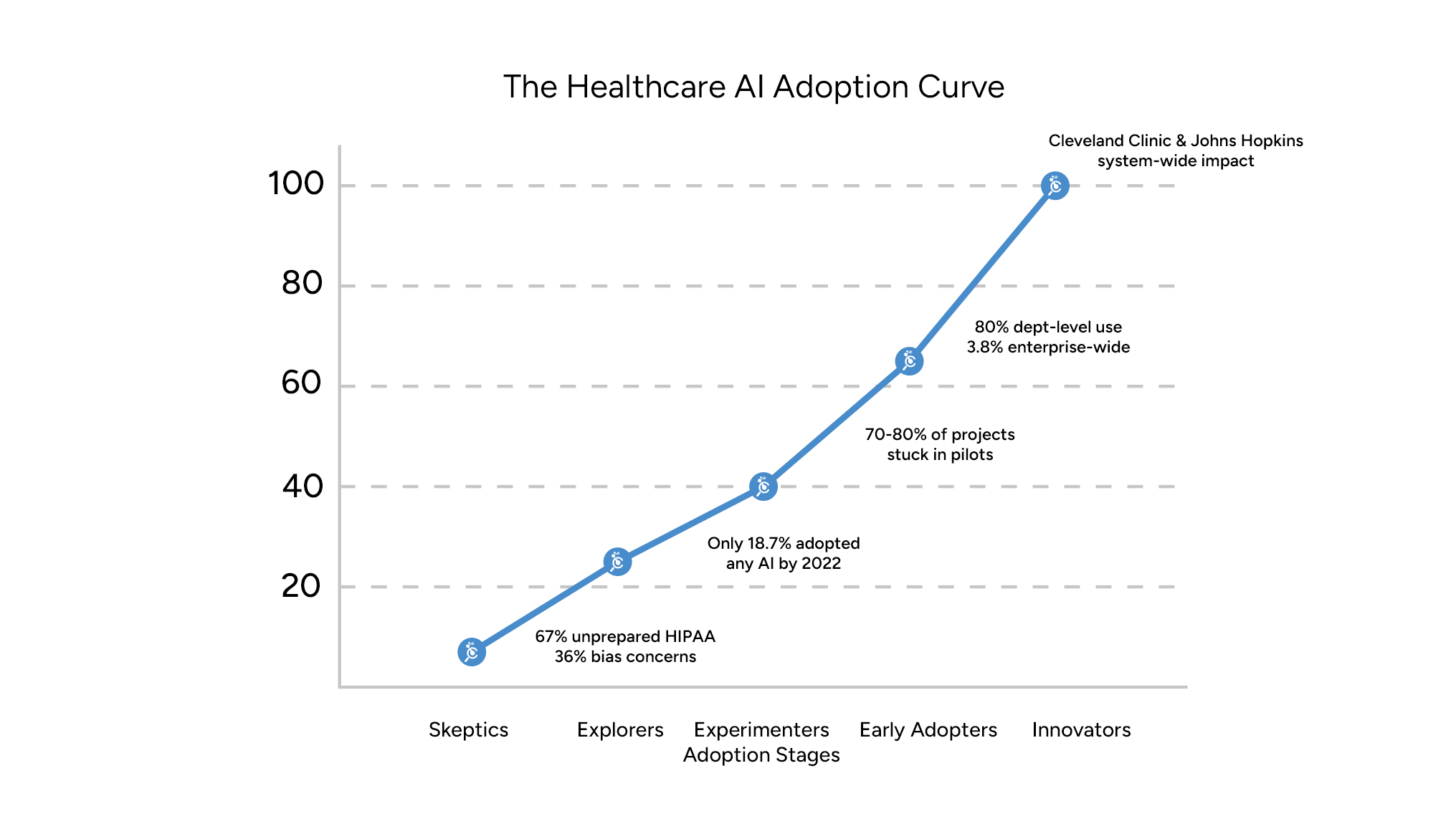
Yet adoption is not a single leap forward. Every practice falls somewhere along the healthcare AI adoption curve. Some remain skeptical of its value, others are researching or running pilots, and a select few have scaled AI across their entire system. Each stage comes with its own opportunities, challenges, and roadblocks. Understanding where your organization stands helps you make smarter choices about what to prioritize next.
The Five Stages of AI Adoption in Healthcare
Skeptics
Skeptics view AI with caution and often see it as risky or unproven. Their concerns center on compliance, HIPAA obligations, and liability if an AI system produces errors. Many worry about vendor overpromises and the lack of clear evidence that AI can improve patient care without adding risk.
Nearly 70% of healthcare executives cite data privacy and security as major barriers to AI adoption, and 36% believe clinical datasets contain too much bias to trust AI for patient care. In addition, 67% of healthcare organizations report being unprepared for evolving HIPAA security standards related to AI. These figures highlight why many organizations remain hesitant to take the first step.
- Roadblocks: Low trust, compliance fears, and cultural resistance from clinicians.
- Path forward: Education and small, low-stakes pilots. Exploring FDA-cleared tools or automating intake workflows provides exposure without putting care at risk.
Explorers
Explorers are curious about AI and eager to understand its potential. They read reports, attend conferences, and meet with vendors. At this stage, leaders see the possibilities but hesitate to act because the options feel overwhelming and the value uncertain.
Despite the high level of interest, adoption has been limited. By 2022, only 18.7% of U.S. hospitals had implemented any form of AI. This statistic underscores the gap between research and real-world deployment, as many organizations linger in an exploratory phase.
- Roadblocks: Information overload, lack of clear ROI, and internal pressure from staff who want relief but fear workflow disruption.
- Path forward: A structured needs assessment. Survey staff about their most pressing administrative burdens—documentation, prior authorization, or billing inefficiencies—and use these insights to focus on quick wins. At this stage, taking an AI readiness assessment quiz can provide valuable benchmarking and help identify realistic first steps.
Experimenters
Experimenters begin moving from theory into practice. They pilot tools in a controlled environment, such as testing an ambient scribe with a handful of clinicians or trying denial prediction software in the billing department. The goal is to see whether AI delivers measurable improvements.
The challenge is that many projects stall. Between 70 and 80% of AI initiatives remain stuck in pilot phases and fail to scale beyond their initial environment. The reasons range from integration issues with EHRs to siloed data that weakens performance, along with inconsistent training or staff buy-in.
- Roadblocks: Technical hurdles, fragmented data, and poorly defined pilot goals.
- Path forward: Establish clear success criteria. For example, aim to reduce documentation time by 30% or lower denial rates by 15% within six months. Involving clinicians, billing teams, and IT staff from the outset builds trust and increases the chance of a pilot evolving into a broader rollout.
Early Adopters
Early adopters expand AI beyond pilots and into multiple workflows. They may implement ambient documentation across the practice, apply predictive analytics to identify patients at risk of readmission, or use automated coding to reduce errors. At this stage, AI becomes part of everyday operations rather than a trial.
Adoption is growing, but true scale remains rare. By 2025, about 80% of hospitals reported using AI in at least one major department to improve patient care or operational efficiency. However, only 3.8% had managed to deploy AI across several departments in a coordinated, enterprise-wide way. This shows that most organizations are still in the early stages of scaling.
- Roadblocks: Rising costs, growing security risks, interoperability issues, and staff fatigue from change.
- Path forward: Formalize governance. Create standards for evaluating tools, track ROI with clinical and financial metrics, and align AI adoption with payer quality programs to ensure value-based care benefits are realized.
Innovators
Innovators are the leaders setting the pace for the industry. They fully embed AI into their systems, using it for clinical decision support, predictive analytics, payer-aligned documentation, and operational efficiency. For them, AI is a strategic advantage as well as a daily utility.
The results can be significant. Cleveland Clinic used AI-driven predictive analytics to optimize patient scheduling, reducing no-shows by 15%, cutting overtime costs by 12%, and improving patient satisfaction by 10%. Johns Hopkins Hospital applied Microsoft Azure AI to automate documentation and lab management, contributing to projected savings in the hundreds of billions across its system.
- Roadblocks: Navigating evolving regulations, ensuring transparency, monitoring for bias, and maintaining clinician trust.
- Path forward: Innovators should share best practices, publish results, and help set industry standards. By contributing their experiences, they strengthen the wider healthcare ecosystem.
AI Adoption in Healthcare is About More Than Technology
Technology itself is not the sole driver of success. Strong foundations matter more. Clean, structured data and interoperable systems are essential for accuracy. Governance frameworks ensure tools are safe, ethical, and compliant. Staff training and payer alignment determine whether adoption truly reduces burden rather than adding new complexity.
AI should be approached as one part of a larger digital transformation. Practices that focus on foundational readiness will achieve sustainable benefits, while those that adopt tools in isolation risk frustration and wasted investment.
Next Steps
Contact us to explore how AI can fit into your workflows.


